UTI Signs, Symptoms, & Antibiotic Treatment For The Elderly
“Wake up! Please wake,” I screamed. There was no response from my otherwise lucid and active Dad. “Let’s take him to the doctor, he has an appointment anyway”, exclaimed his wife anxiously. Quickly, I answered her, “There is no way we can take him to the doctor now, he is not responding.” I must call an ambulance”. “By the way” I asked, “Why is he going to the doctor?”
His wife answered immediately, “He was complaining about pain while urinating.” Beware, a sudden change in behavior in the elderly can be a sign of a UTI (urinary tract infection). Besides for the pain that comes with a UTI, bladder infection signs can be also notice from a change in an adult’s comportment.
With my sister’s agreement, I quickly called an ambulance and my Dad was taken to the hospital and diagnosed with an acute UTI.
UTIs are quite common in older adults but there is a disagreement among medical specialists when to treat this ailment with antibiotics and when to forgo this medicine.
The introduction of antibiotics is one of the greatest achievements in modern medicine. Early in the 1900’s, many sick Americans died due to various infections. Alexander Fleming, a Scottish physician, during the 1920’s, isolated an active substance in a mold that had contaminated bacterial samples in his laboratory. Interestingly, the contaminated bacteria seemed to be dying off due to the mold. The active substance causing the destruction of the bacteria was isolated by Dr. Fleming naming it “Penicillin”. This antibiotic changed the role of infection in modern day medicine.
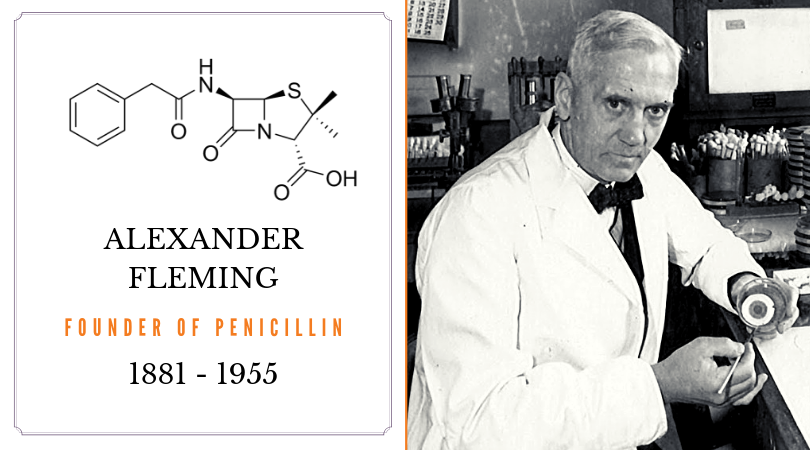
In the year, 1928, Fleming began experimenting with the influenza virus in his lab at St. Mary’s Hospital in London. After returning from a two-week vacation, Fleming found that a mold had formed on an accidentally contaminated staphylococcus culture dish. On closer examination, he realized that this culture had prevented the growth of the staphylococci. He described this mold colony as a fluffy white mass increasing in size after a few days and changing colors from dark green to black to bright yellow.
Selman Waksman, in another laboratory in New Jersey (a few years later), developed another antibiotic named streptomycin which was the first effective treatment for tuberculosis. Prior to this antibiotic treatment, tuberculosis or TB was not curable. Lucky, affluent individuals and children were sent to the Swiss Alps to enjoy and breathe in the fresh mountain air which could sometimes save their lives but not necessarily alleviate all the symptoms.
As more antibiotics were discovered, the life expectancy in the United States increased as death from bacterial infections began to decline.
In both their acceptance speeches for the Nobel Prizes in 1945 and 1952, Fleming and Waksman, both warned that eventually in the future their work might be crippled because of antibiotic resistance which will cause the revival of deadly infections.
Although there are well over 100 antibiotics, the majority come from only a few types of drugs.
These are the main classes of antibiotics.
1) Penicillins such as penicillin and amoxicillin
2) Cephalosporins such as cephalexin (Keflex)
3) Macrolides such as erythromycin (E-Mycin), clarithromycin (Biaxin), and azithromycin (Zithromax)
4) Fluoroquinolones such as ciprofloxacin (Cipro), levofloxacin (Levaquin), and ofloxacin (Floxin)
5) Sulfonamides such as co-trimoxazole (Bactrim) and trimethoprim (Proloprim)
6) Tetracyclines such as tetracycline (Sumycin, Panmycin) and doxycycline (Vibramycin)
7) Aminoglycosides such as gentamicin (Garamycin) and tobramycin (Tobrex)
The overuse of antibiotics is the main cause of drug resistance. Complex mutations can develop from bacteria that normally vegetate in the human body. As the susceptible bacteria are killed off by the antibiotic drug, resistant ones are left behind to multiply. One person can be in danger of being colonized by several different species of bacteria.
On March 15, 2019, Paula Span, from The New York Times, stated that in a new CDC (Centers for Disease Control and Prevention) study, older people are taking too many antibiotics. Patients over sixty-five years of age, have the highest rate of outpatient prescriptions; more than any other group. (Pediatricians are one group of healthcare practitioners who are on the forefront of a major reduction of antibiotic prescriptions.) The CDC study written up in the Journal of the American Geriatrics Society, indicates that in 2014, doctors wrote nearly fifty-two billion antibiotic prescriptions. This means enough for every older person to get a least one. This is not even including hospitals, nursing homes and long-term acute care facilities.

Dangerously, these drug resistant bacteria, can spread in hospitals and nursing homes through un-sterile surfaces or careless health-care workers. If one patient carries a resistant bacterium, it can cause a major outbreak in a healthcare facility. For example, at the National Institute of Health Clinical Center, eighteen patients were affected with a CRE (carbapenem resistant enterobacteriaceae bacteria). An alarming six patients died.
There are several different types (classes) of antibiotics used to cure UTI infections in the elderly.
1) Quinolones are quite strong and can have major side effects – more than initially realized by the FDA. Noroxin, Maxaquin, Levaquin and Cipro are some of the most popular ones. Some of the side effects of this class of antibiotics are:
- Changes in blood sugar levels which can be dangerous for diabetics.
- Neuropathy (nerve damage which causes both numbness and pain)
- Arrhythmia (an irregular, fast or slow heart rate)
- Nausea, insomnia, anxiety disorders
- Tendinitis and tendon rupture
These drugs should be used cautiously by physicians. Unfortunately, use of fluoroquinolones is widespread with one in three patients given it unnecessary. One patient, I know personally was given Cipro after prostate surgery. After aggressive vomiting could not be explained by the surgical team, his own physician diagnosed an allergic reaction to Cipro and advised the patient to stop taking it immediately. The vomiting stopped right away. How did this physician know more than the surgical team? Only because he had once had the same reaction to Cipro himself.
Patients pressure their health care providers, causing doctors to give in and prescribe these medications for varied medical conditions such as flu and other viral infections which do not require such medical intervention.
2) Nitrofurantoin (Macrobid, Macrodantin) are also frequently used for the symptoms of UTI. For uncomplicated cases this class of drugs should be tried first. Nitrofurantoin can be prescribed as a one pill daily long-term fix for frequent UTI infections.
The term, UTI can be an unclear and often overused diagnosis when older adults have no physical symptoms except a doctor’s visit and urine test which shows bacteria in their urine. Some researchers are coming to a new understanding that some bacteria live in the human body naturally. However, we cautiously prevail on you to make sure to always check any symptoms with your doctor. If you do have symptoms such as the ones described above, it is vital to get immediate medical attention. Always take the cautious route. Neglecting a UTI can cause a serious blood stream infection called, sepsis.
Women are more likely than men to experience UTI’s because of the difference in the anatomy of men and women. Seniors are susceptible to UTI’s for several reasons. Firstly, their immune systems are weakened. Secondly, seniors have a decreased awareness of self-care.
Antibiotics were developed to save lives and cure infections. There is a much lower likelihood of dying of infection today than in the days prior to antibiotic therapy. However, the life expectancy for England and the United States have begun to fall and in England it has been partially attributed to antibiotic resistance increase.
Physicians and patients must begin to be more critical about the role of antibiotics as patients get older. By thinking about long term effectiveness instead of just immediate relief, patients will continue to benefit from receiving antibiotics. This writer is of the opinion that the use of antibiotics in older adults should not be curtailed but rather it is vital that a patient and/or his caregiver monitor the antibiotic use for side effects. If the patient begins to feel worse instead of better, you can suspect that he is having an adverse reaction to the medication. However, do not stop it without your physician’s approval. As you see above there are a variety of antibiotic options. No one would want their loved one to contract a dangerous blood infection which would require hospitalization. Bear in mind that advocates of limiting antibiotic use are clearly discussing the times that a patient goes to the doctor for something else and the doctor notices only a minor abnormality in the urine specimen. If the patient has specific symptoms of a UTI, including but not conclusive of the symptoms below, there is a good chance that antibiotic therapy will be essential and crucial.
For a quick reference, here are some of UTI symptoms:
- urethral burning with urination.
- pelvic pain.
- frequent urination.
- an urgent need to urinate.
- a fever.
- chills.
- urine with an abnormal odor
